Learning Disabilities and Visual Impairment
A post dedicated to Sally
Today's post is dedicated to a patient of ours - Sally, who sadly passed away during the Covid-19 pandemic.
Sally needed glasses since she was a child, but was always reluctant to wear them. No one ever noticed any other sight problems until she was 26/27 years old when she started to rub her eyes constantly and started to describe an 'itch' on her head. She visited the GP a couple times but nothing was ever mentioned about any sight problems. A few months later, the family noticed that Sally was having some issues with her vision and called a domiciliary optometrist to have her eyes checked, when they found out that Sally had extremely high pressures in her eyes. She was diagnosed with Glaucoma and despite the aftercare that helped lowering her eye pressures, Sally lost almost all her vision, only being able to differentiate between light and dark. Since then Mom - Maureen, tried to bring awareness and better access to regular eye health check-ups for people with learning disabilities.
Our Resident Optometrist, Jig Joshi wrote a few words about that matter:
“Sally & Maureen Rose were vital to the inception of our local service and through this Learning Disabilities Enhanced Optometry Service (Bridge to Vision), we managed to identify adults with vision problems and help them in various different ways to improve, maximise or maintain their eye health and vision. Often it was about making sure people got the specialist eye care they needed from their optometrist and the correct treatment such as glasses, along with support to wear them. It really helped for people to have familiarity and consistency of who they see for their eye care, and to feel comfortable in their surroundings."
You can read the full story and Jig's full Testimony at: https://www.seeability.org/news/sallys-legacy
Sally's story makes us wonder how much do we really know about patients with Learning Disabilities and Visual Impairment and how these two are related.
What causes Learning Disability?
The main causes of LD in the United Kingdom are:
- Prematurity;
- Chromosomal disorders;
- Cerebral Palsy;
- Genetic Disorders;
- Metabolic Disorders;
- Toxins (alcohol, drugs, iatrogenic).
What do we mean by Learning Disability?
When we say Learning Disability, we are talking about patients who experience:
- Significant reduced ability to understand new/or complex information and/or skills;
- Reduced ability to cope independently (socially impaired functioning).
This happens before adulthood, with a lasting effect on someone's development, meaning that patients with learning disability will have difficulties in understanding, learning new things and socialising with other people in general. Of course this variants depend on the extend and nature of the disability itself.
Visual Impairment and Learning Disability
The main causes for Visual Impairment in patients with LD are:
- Refractive error;
- Amblyopia;
- Strabismus;
- Congenital Cataract;
- Nystagmus;
- Corneal Problems;
- Optic pathway abnormalities;
- Perceptive and interpretive problems.
According to https://www.learningdisabilities.org.uk/
there are approximately 1.5 million people in the UK with a LD. Patients with a LD may not know that they have a visual problem or may not be able to tell others about it.
Statistics from https://www.rnib.org.uk
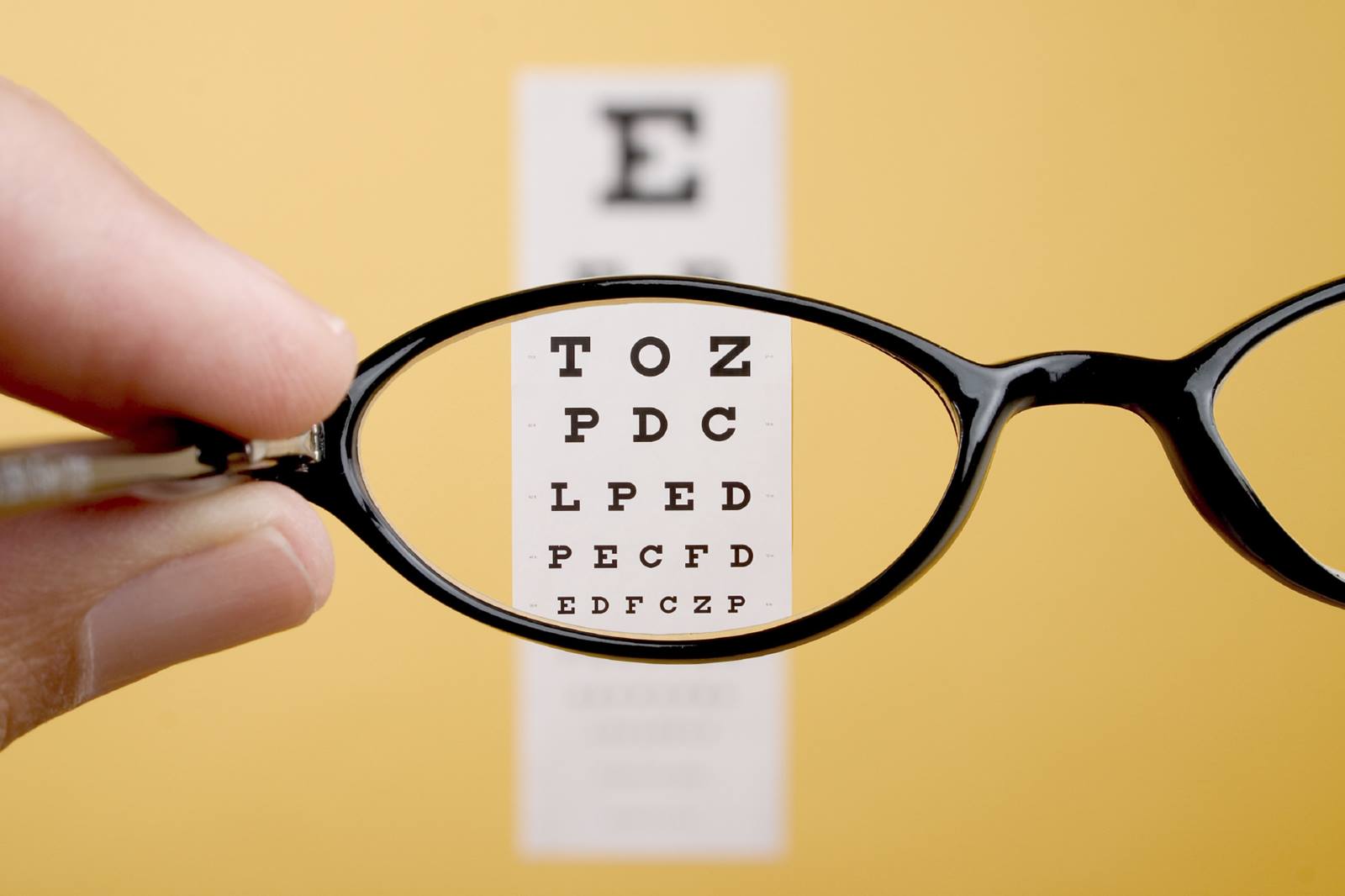
fact that there are 96,500 adults with a LD who are blind or partially sighted as a result of an eye condition (Cataract or Squint), health conditions (as Diabetes), normal aging of the eye or any other eye conditions associated with LD. It is important to know that patients with LD are 10 times more likely to have serious visual problems, which is normally more severe within patients with profound LD. 6 in 10 people with LD need glasses and often need support to get used to them.
Visual problems can also affect patients with LD in many ways, such as:
- Social isolation: Sight helps people to take part in the world surrounding them. When they experience a visual impairment, because the vision is compromised, these patients tend to get excluded from certain situations or they may even isolate themselves, as they are not aware of what is going on around them;
- Motivation: Poor/low vision may reduce someone's motivation to discover more of their surroundings. Patients with LD often seem to be lacking 'drive' and lack of will to do and control more. Patients who have not learned how to control their environment may appear compliant and passive;
- Communication and Behaviour: As low/poor vision affects the ability to make eye contact, understanding facial expression, body language and gestures, as well as learning and using sign language, this makes it difficult for the visual impaired to communicate with others or to understand communication through facial expression;
- Co-ordinating other senses: Patients with a Visual Impairment and LD take longer to explore and complete tasks as they will find hard to understand the world surrounding them and to predict the actions of others around them. Vision helps us to understand what we hear, touch or taste, helps us to predict and anticipate what's coming and how to react.
What symptoms should we look out for?
Some unusual behaviour might happen as a strategy to cope with a vision loss or an attempt to make the most out of it. Some possible symptoms are:
- Becoming withdrawn or uncommunicative;
- Being clumsy and/or falling more;
- Rocking, head shaking or flapping their hands;
- Holding things really close up;
- Rubbing and poking the eyes;
- Feeling confused or disorientated;
- Startled by noised or people approaching.
If these or any other similar symptoms that were never seen before suddenly start to happen, please make sure to book an appointment with an LD Specialist Optometrist. Patients with LD should have at least one eye examination every 2 years, just to make sure there are no significant changes in their eyesight.
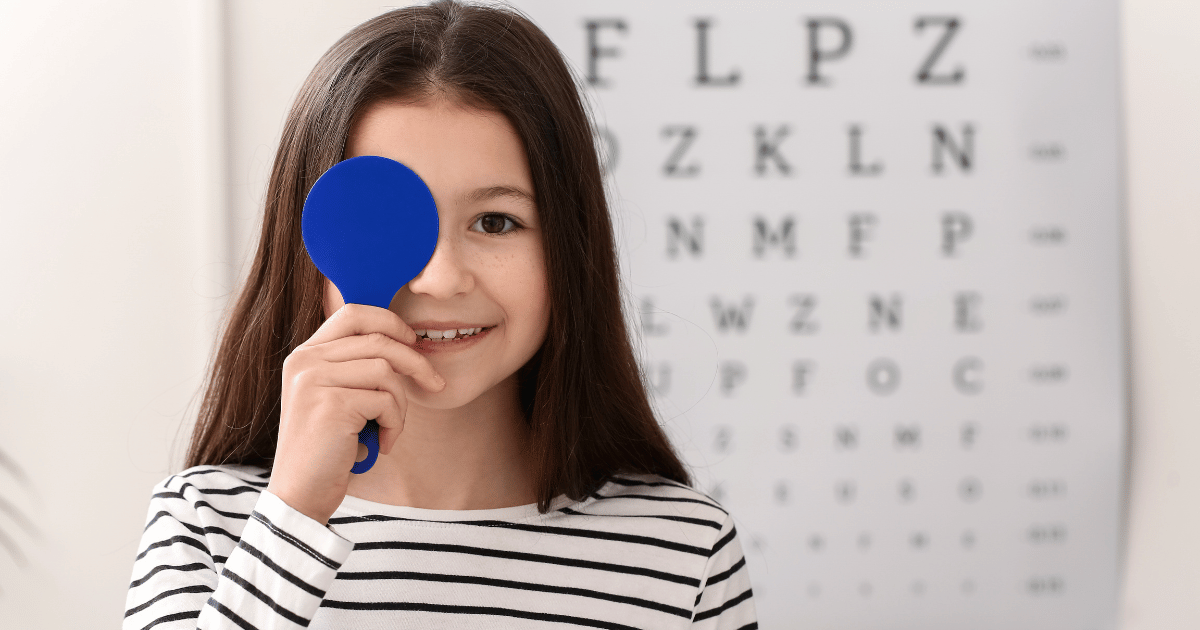
Will the test be difficult for them?
Parents, relatives and carers often feel that due to their disability, it might not be possible to carry a full eye examination. With the proper equipment, training and some alternative tests and approaches the Optometrist will be able to adjust to the patient's needs and to deliver a full eye examination.
In both Woodford & Dagenham practices we are equipped and trained to examine patients with LD. If you feel like your child or the person you are caring for is experiencing any of these symptoms above, or if they have a LD and never had an Eye Examination before, it would be a good idea to have them tested. To book an appointment, please call or email us and we will be more than happy to help you with that.
Keep in mind that at Care Optics - Eye care, We Care